Addiction Psychology Explained?
Addiction is fundamentally a brain disorder – but it’s not just about biology, with a substantial number of psychological and psychosocial factors playing a crucial role in the development and maintenance of addiction.
What is the Psychology of Addiction?
The transformation of a habit into an addiction is a process deeply rooted in the brain’s response to behaviour. When an activity is perceived as rewarding, the brain’s reward system is stimulated, releasing chemicals like dopamine that create an urge to repeat the behaviour for its inherent pleasure or rewards. Repeated engagement in such behaviour strengthens the desire to continue it, driven by the dopamine-induced positive sensations and the aversion to the negative feelings arising from its absence. Thus, a routine habit can gradually escalate into an addiction, with the reward system becoming increasingly disordered, compelling the individual to sustain the addictive behaviour in pursuit of neurochemical balance.

How can a habit become an addiction?
Our understanding of behavioural addiction is still evolving, and while comprehensive diagnostic models are yet to be established, the reality of behavioural addictions as genuine addictions is undeniable. This perspective is supported by substantial neurological evidence. The American Society of Addiction Medicine, a foremost international authority on addiction, clarifies that addiction concerns brain functionality and circuitry. It highlights the fundamental differences in the brains of those with addiction compared to those without. Consequently, behavioural addiction is a distinct disorder in its own right, demanding a coherent treatment approach akin to that for drug addiction, despite the absence of any external physical substance causing dependency.
The Disease Model of Addiction Versus
The Choice Model of Addiction?
Psychologists studying addiction have generally aligned with two camps: the disease model and the choice model of addiction.
The disease model posits that addiction is a disease, potentially rooted in biology, genetics, or environmental factors. This perspective suggests that changes in the brain, particularly in the mesolimbic pathway, are central to addiction, independent of the individual’s conscious choices. Proponents of this model often believe in the possibility of a pharmaceutical or surgical solution to addiction, which could “heal” the affected brain areas and eliminate the compulsion for addictive behaviour.
Conversely, the choice model assigns responsibility for addiction to the individual. It argues that addiction stems from the deliberate decision to engage in addictive behaviours repeatedly, despite understanding the negative consequences. Supporters of this model generally reject the idea of a pharmaceutical or surgical cure for addiction, emphasising instead the need for behavioural change and conscious decision-making to achieve and maintain abstinence.

Fast Access to Residential Treatment
We are currently able to offer fast access to private inpatient treatment.
Please call us today and speak to one of our expert advisors.
Call today in confidence: 0800 0148 970
Individual Differences and Susceptibility to Addiction
It’s a well-acknowledged fact that not everyone is equally prone to addiction. The scientists continues to debate why certain individuals fall prey to addiction while others remain unaffected. However, there are several identified factors that significantly contribute to the risk of developing an addictive disorder.
Genetic
Addiction is often seen running in families, pointing towards a hereditary component. One of the most significant indicators of a person’s risk for addiction is their family history. The genetic underpinnings of addiction are increasingly being understood, particularly the role of DeltaFosB overexpression in the mesolimbic pathway, which is a common thread in nearly all addiction cases.
Personality disorders
Personality disorders are conditions that significantly impair personal and interpersonal functioning and are not attributable to a medical disorder. These disorders are often linked to an increased likelihood of addiction, particularly substance addiction. This could be because individuals with these disorders may be trying to ease their psychological burden. They might also use substances as a way to cope with feelings of worthlessness or to combat difficulties in social interactions.

Though no one can go back and make a
brand-new start, anyone can start from
now and make a brand-new ending
Psychological coping strategies
Stress and trauma are significant triggers leading many to substance abuse or engaging in other immediately gratifying but potentially harmful behaviours. These actions can quickly become addictive. Individuals grappling with these issues might increasingly turn to these behaviours, more frequently and intensely than usual, as a means of distraction or escape from their difficulties.
Mental disorders and addiction
There’s often a close relationship between mental disorders and addiction. Some mental disorders directly lead to compulsive behaviour, which can easily become addictive. Other disorders might encourage addictive behaviour (particularly substance abuse) as a form of self-medication or escapism for life situations. Addiction can also be a consequence of these mental disorders.
Dual diagnosis and addiction
Encountering a substance use disorder alongside another mental health disorder is commonly referred to as a dual diagnosis. This co-occurrence is notably prevalent in addiction cases. Dual diagnosis invariably complicates the treatment process, as it necessitates simultaneous management of both conditions. Moreover, the treatment for one disorder can often adversely impact the management of the other, further entangling the situation.

Psychological Mechanisms of Addiction
The path to addiction is often paved with various psychological mechanisms. Understanding these underlying processes is crucial in addressing addiction effectively.
Rebound effect
The rebound effect is what happens when symptoms that were controlled by medication or drug use come back, often worse, after stopping the drug. For instance, a person who uses medicine for insomnia might find themselves having even more trouble sleeping after they stop taking it. This effect is a big reason why people get addicted; they feel they need to keep using the drug to avoid these worse symptoms. The rebound effect is also a common part of withdrawal.
Reinforcement
“Reinforcement” in behavioural psychology signifies the process whereby a behavioural response is incrementally strengthened when followed by a specific stimulus. Both positive and negative reinforcements play critical roles in fostering addiction, with positive reinforcement being more typical. This is characterised by the pleasurable sensations and experiences stemming from substance abuse, which individuals repeatedly seek, thereby fuelling continual substance misuse.
Reward system
Sensitisation is a phenomenon where repeated exposure to a certain stimulus gradually amplifies the response to that stimulus over time. For example, the initial experience of gambling might elicit a certain level of enjoyment. However, continuous engagement in gambling can lead to an increased sensitivity to this activity, resulting in a more intense and heightened response with each occurrence. This concept is not confined to behavioural addictions like gambling, it also extends to substance abuse. In the context of drugs, sensitisation means experiencing progressively stronger effects with each subsequent use.
Sensitisation
The reward system is a term for brain segments that dictate motivation, desire, and cravings, influencing our inclination towards or against certain behaviours. This system encompasses numerous interconnected brain areas and structures, and any anomalies in these areas can trigger compulsive addictive behaviours. Primarily, addiction is fundamentally a disorder of this reward system, although there is still a lack of common agreement among scientists and psychologists about the specific nature of this disorder’s development.
Brain Structures, Hormones and Addiction
Numerous brain parts and hormones, which act both within and upon them, play a critical role in the development of addiction.
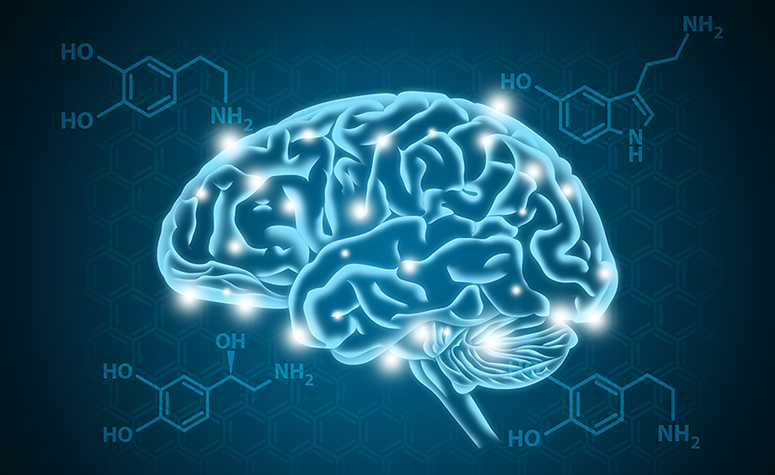
Dopamine and addiction
Dopamine, a crucial hormone and neurotransmitter, fulfils several vital functions in the human body, notably influencing motivational salience (the drive to undertake or avoid specific actions). Commonly referred to as a “pleasure chemical”, dopamine more accurately triggers reward-related feelings rather than pure pleasure. The anticipation of a reward elevates dopamine levels, thereby fostering a yearning for that reward. Many addictive substances either heighten dopamine release or hinder its reabsorption, impacting the body’s system. A lack of dopamine can lead to unpleasant sensations and emotions, which in turn escalates addictive behaviour.
Nucleus accumbens
Located in the basal forebrain, towards the front and lower part of the brain, the nucleus accumbens is a vital component of the ventral striatum, which it forms alongside the olfactory tubercle. This brain region is intimately connected with motivation and reward, playing a significant role in the experience of pleasure. It’s the endpoint of the mesolimbic pathway, receiving projections from dopamine-conveying neurons. The over expression of the gene transcription factor DeltaFosB in the nucleus accumbens is now seen as the primary mechanism behind the result of addiction, whether that be behavioural or substance-related addiction.
Serotonin
Serotonin, a neurotransmitter, is often associated with fostering feelings of joy, contentment, and gratification. However, its role is considerably more intricate, encompassing aspects of reward, memory, cognition, and learning, alongside governing several physiological functions like appetite, mood, and sleep regulation. Various substances of abuse, including a selection of psychedelic hallucinogens, enhance serotonin production, as do certain antidepressants. The pursuit of the euphoric sensations linked to serotonin can lead to addictive behaviours. Similarly, the urge to escape the adverse effects of serotonin shortage, particularly following substance misuse, can also contribute to addiction.
Neuroplasticity
Neuroplasticity refers to the brain’s capacity to adapt and change throughout a person’s life. This includes variations in the amount of grey matter and the potency of certain neural connections. Habitual engagement in addictive behaviours can lead to structural modifications in key brain parts, thereby reinforcing addiction and complicating recovery efforts. Similarly, specific forms of substance abuse can promote neuroplastic changes, not only reinforcing addiction but also potentially leading to detrimental long-term effects, such as cognitive decline.

Fast Access to Residential Treatment
We are currently able to offer fast access to private inpatient treatment.
Please call us today and speak to one of our expert advisors.
Call today in confidence: 0800 0148 970
Addiction Psychology and Dependence
The concept of psychological dependence revolves around an individual’s reliance on a particular substance or behaviour for normal psychological functioning. This type of dependence is characterised by the emergence of psychological withdrawal symptoms when the individual ceases using the substance or engaging in the behaviour. Over time, as a person consistently partakes in a specific activity or substance use, they undergo a psychological adjustment to the effects of this repeated experience, which can encompass substance abuse.
Psychological dependence, while intimately related to, is distinct from the broader phenomenon of addiction. It often plays a contributory role in the development of addiction, as individuals afflicted by it feel compelled to continuously engage in substance abuse or other addictive behaviours. This compulsion is a means to avoid or alleviate the discomforting psychological symptoms experienced during withdrawal. It’s important to distinguish psychological dependence from physical dependence, as they differ in the nature of their withdrawal symptoms. However, they often co-occur, and in some instances, psychological dependence can manifest physical symptoms psychosomatically.
Treating psychological dependence typically involves a combination of detoxification and psychotherapy. Detoxification is the initial step, addressing the immediate effects of withdrawal. It’s essential for stabilising the individual, setting the stage for the more in-depth treatment that follows. Post-detoxification, psychotherapy becomes crucial. This stage focuses on altering the behavioural patterns and thought processes underlying the dependence. In certain situations, ongoing pharmaceutical management might be necessary to effectively manage withdrawal symptoms.

Modalities of Treatment for Addiction
Addressing the global epidemic of addiction, particularly to alcohol and drugs, is now a priority in public health. The treatment of addiction has evolved into a sophisticated field, driven by ongoing research into various facets of this complex phenomenon. Diverse treatment approaches, grounded in different philosophical perspectives, are offered by public, private, and third-sector organisations worldwide.
The contemporary consensus in addiction treatment combines detoxification and psychotherapy, often supported by medication. The most effective approach is generally agreed to be residential rehabilitation, where individuals stay in a dedicated facility. However, other formats also prove successful in many cases.
The journey to recovery from addiction is often a protracted and lifelong endeavour, extending well beyond the initial treatment phase. In support of this enduring journey, numerous global organisations offer ongoing assistance to individuals in recovery, beyond the structured environment of a treatment programme.
Recovery from addiction is typically a long-term journey, extending well beyond the initial treatment programme. Numerous organisations worldwide support recovering addicts outside the traditional treatment environment.
- Detoxification and Medically Managed Withdrawal
- Long-Term Residential
- Short-Term Residential
- Individualised Drug Counselling
- Group Counselling
- Intensive Outpatient Program (IOP)
- Outpatient Treatment Programme

Benefits of Addiction Treatment and Rehab Centres
Residential rehabilitation, commonly referred to as “rehab,” is widely recognised as the most effective form of treatment for addiction. In such a setting, addicts reside within the facility, typically for a duration ranging from 30 to 90 days. Though this period can significantly vary depending on each individual case, with primary purpose to undergo treatment in a secure, peaceful, confidential, and substance-free environment, all thoughtfully designed to foster healing.
The key advantage for addicts in rehab is the constant availability of medical professionals, who possess extensive experience in addiction treatment. This round-the-clock presence of healthcare experts ensures that any medical needs are promptly and effectively addressed. Additionally, being in the company of fellow recovering addicts offers not just moral support but also invaluable advice and the simple yet profound benefit of companionship.
Rehab centres usually split the treatment into two main phases: detoxification and the subsequent rehabilitation phase, with therapy being the cornerstone of the latter. The detox phase focuses on the physical aspects of addiction, while rehabilitation delves into therapeutic interventions to address the psychological dependencies. A critical component of this approach is the provision of up to a year’s free aftercare for clients post-treatment, boosting the chances of a successful and sustained recovery.
Addiction Psychology and Counselling
Counselling plays a pivotal role during both the addiction treatment and the ongoing recovery process. It addresses specific challenges, and for many individuals battling addiction, counselling can be a lifesaver. This is particularly true in the initial stages of treatment when individuals are often grappling with the overwhelming psychological impact of addiction.
In rehab settings, counselling is usually provided alongside psychotherapy. However, addiction counsellors are also available outside rehab environments. Many recovering addicts continue to engage in counselling long after leaving a clinic, as it supports them throughout their recovery journey.
FREE Addiction Assessment
If you or a loved one are struggling with addiction, we understand the challenges you’re facing and we’re here to offer compassionate help.
Our highly trained advisers are available to speak to you right away, simply call 0808 252 3379 today.
We can discuss your concerns in complete confidence, explore the options for treatment, and help you to understand what will work best for you.
We’ll also help you to book your free addiction assessment there and then, with appointments usually available within only a few days.
We understand that taking the first step can be the most difficult, but we’re here to support – with no pressure or judgement.
Professional and compassionate help is just a phone call or click away.